Commercial Determinants of Health (1). Introductory thoughts
Commercial
Determinants of Health
This is the first in a series of blogs on the commercial determinants of health. Other blogs in the series
1. What is the issue, what is it all about - this one
2. The neoliberal framework into whichthis fits
3. Tactics used by industry
4. Counter tactics used by public health
Firstly … what is it all about
1 What’s it all
about
Take tobacco as
an example – cause of 20% of deaths about 15% of all illness. Other things are
rapidly catching up like obesity and alcohol related illness and death. All up
non communicable Diseases continue to kill 41 million people world wide and
account for 70% of all deaths.
One can argue
that at the centre of this toll is the collective of individual lifesely
choices made by all of us. Equally one can argue that at the heart of each of
these issues are organisations who want to sell products and services and
maximise profits for their shareholders.
Profit-seeking
businesses engage in promotional activity, which harms society as it increases
the consumption of unhealthy commodities. Often the commercial interests at the
heat of this will portray virtue and
individual choice but are really promoting harm. They do not change their
tactics unless regulation forces the hand – e.g. how tobacco industry operates
in UK vs less well off countries.
Thus the actions of these commercial interests
(and the wider supply chain) in shaping an environment that maximises sales
determines, in part at least, the patterns of behaviour of whole populations to
consume. The consequence of that behaviour can be expressed in health terms or
in environment terms. That is the essence of framing the commercial
determinants of health. Just as we think of the “social determinants” as an
alternative to framing a health issue as one of individual responsibility and
treatment, so should we consider the actions of industries.
WHO have
published an excellent piece on the Commercial Determinants of Health. Commercial determinants of health
are the private sector activities that affect people’s health positively or
negatively. WHO frames it widely in terms of the impact of the private sector choices
on social, physical and cultural environments through business actions and
societal engagements; for example, supply chains, labour conditions, product
design and packaging, research funding, lobbying, preference shaping and
others. These company choices then impact on individual and planetary health.
There is no doubt that the private sector makes many positive contributions to
public health, it is not a one sided argument.
2 Framing. Whose
responsibility is it anyway
The concept of
the “commercial determinants of health” goes to the heart of our approach to
public health policy. Namely and most specifically whether interventions are framed
as a matter of “individual responsibility” and “freedom of choice” or whether
interventions are shaped in the context of commercial social and economic
drivers that determine our behaviour.
This is then
further exacerbated by setting and framing some public health issues from the
perspective of the individual, the choices they make and the psychological
drivers of this. A topical example at the moment is gambling harm which has
been seen through the frame of psychiatry, psychology, and the neurosciences with
a focus on the individual gambler. This isnt inherently wrong, but it CAN
divert attention of policy makers (toward thinking answers can be at individual
level) and individual approaches couched in personal responsibly are in no way
sufficient and overlooks the social and political processes and harmful
business practices, products, and policies in which policy is set.
It took decades
of effort (and it is still unfinished business) to shift the dial of narrative
on obesity away from the person making “poor” lifestyle choices toward the
context into which people make those choices. There is STILL a long way to go
on that one. We are continually being drawn back into individualistic narrative
and interventions.
We can (and
should) choose to help individuals change behaviour for example investment in
smoking cessation service is spectacularly effective and cost-effective things
to do do but it makes little difference to population prevalence. Thus we should also frame our interventions in shaping
the right social economic and commercial environments that enable the healthy
choice to be easiest. Put most bluntly this is about the regulation of
industries to curb sales of products that have harmful effects. An approach
framed around regulation is often not in keeping with the interests of
commercial organisations that benefit from selling us too much of a certain
product or service. That’s where the pushback starts.
3 these things can come and go in cycles and we shouldn’t neglect
the lessons of history
There are well
documented strategies and tactics that undermine effective public health
policies, including framing the issue as one of individual responsibility, not
requiring regulatory action. Thus the core role for public health is to make
the case comprehensive strategies to tackle these epidemics of consumption,
including effective regulation, in the face of policy interference from vested
interests.
See for example Briggs on why getting
this stuff right and not forgetting decades of advocacy on tobacco control
matters. This was in the context of research, but there are many parallels with
policy formation and implementation
·
Letting industry “in” lends
the industry legitimacy and status—giving (or the perception of giving) industry-sponsored
research a false equivalence with independent, credible, public health research
·
industry participation at academic conferences and other
scientific arenas provides critical insight into tobacco control evidence and
strategy, which the industry can then use to counter science-based policy
initiatives
·
legitimizing tobacco industry findings allows them to showcase
their work to federal regulators.
·
younger researchers may not be aware of the tobacco industry’s
long history of dishonesty and therefore may be less likely to appreciate the
consequences of industry participation in scientific forums. Lessons learned
from decades of deception by the tobacco industry should not have to be
repeated
·
this may be particularly true among America’s youth or those who
have simply forgotten the industry’s egregious reputation and their ongoing
unethical practices
·
By appropriating the language of harm reduction, the tobacco
industry cynically claims to care about users’ health
·
By participating in legitimate scientific activities, the
tobacco industry gains the imprimatur of integrity—a veil that is increasingly
being taken at face value
·
all serve to shift public perceptions of the tobacco industry,
subtly directing the general public into believing the industry’s pretence that
it can be part of the public health solution to end smoking
·
There is no indication that their motivations have changed—their
goal remains the expansion of their market share for nicotine addiction
regardless of the public health consequences.
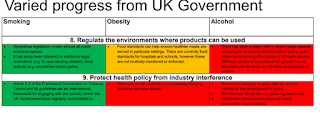
4 How much progress is being made on things framed as CDOH
Progress from UK Govt is varied across some of the areas
commonly framed as CDOH. See a suggested report
card here (from a recent Yorkshire conference)
My sense is c minus overall and for alcohol especially in
England a “see me after class” rating. Of note gambling harm wasn’t on this
assessment.
There are many writing about strategies framed in a CDOH
model of thinking. See for example the Obesity
Health Alliance 10 year healthy weight strategy. This is not framed around
“individuals” and “weight management”, it is very well framed in regulatory and
addressing commercial determinants
5 why ONLY focusing on policies isn’t enough. The industry IS the issue
One, important in
my view, critique of a great deal of the current work is that whilst some of
these policies are very welcome and will be impactful, often the is a
disconnect with the fundamental nature of the tactics of the industries such
policies are seeking to address. See
for example on this on low / no alcohol - The-Marketing-and-Consumption-of-No-and-Low-Alcohol-Drinks-in-the-UK-March-2022.pdf
(ias.org.uk). One could frame this as a harm reduction product or a trojan horse
towards further normalisation in new cohorts. Harm reduction in the space of
tobacco (vape / heat not burn) has divided the PH community. Much rests on our
ability to regulate (and resourcing to enable this) and who harm reduction
products are marketed to. A glass half
full approach might conclude that such harm reduction products are representing
an effort from industry to grow a new market. For low / no alcohol it
might be easy to see a scenario of all the marketing tactics on alcopops all
over again. It IS possible to see many parallels to tobacco owned vapes which
are being aggressively marketed in ways that appeal to young people. There are
obvious fears on normalisation, gateway to more harmful products. Obviously
opproach on regulation is key (and I need to emphasise that regulation needs
national policy and resource to actually implement), but also being savvy to
the commercial drives and willingless to think about the specific policy in
that light not just a policy in isolation.
The critical issue and the heart of it – it is the nature of the product and the tactics and nature of industry that should be the focus
The critical
issue with regard to the commercial determinants of health is that it is the
nature of the product and the practice of the industry that sells the product
harmful to our health that is the issue, and thus the target of intervention.
The thorny issue of private profit versus public health
Companies seek
profits. That is that their shareholders expect them to do, rightly. However
the profit-seeking nature tends to encourage and incentivise businesses to engage in promotional activity, which can
harm society as it increases the consumption of unhealthy (to humans or to the
planet) commodities. Thus the essence of the CDOH oriented approach is that to
curb these industrially driven epidemics we need regulatory frameworks that
moderate the behaviour of businesses and work to protect public health.
The next blog in
the series will consider the neoliberal framework in which CDOH sits



Comments
Post a Comment